Everything you need to know about stem cells
What are stem cells, and what makes them so unique? What are the different types of stem cells, and how have they impacted modern medical science? Here is us answering all your questions about stem cells.
If you lived in the 17th century, what do you think would have been the average human life expectancy? 60 years?… 70 years? As a matter of fact the number was way lesser, somewhere between 30-40 years, based on the region. This number should not be surprising considering the kind of infectious diseases doing rounds at that time. Smallpox, plague, typhoid, cholera, leprosy, to name a few, periodically hit the masses. They killed thousands to millions each time. Bubonic plague is known to have wiped out nearly one-third the world population back in the 1300s. The hopeless devastation caused by these infectious microorganisms was indeed dreadful.
However as of today we have almost doubled our life expectancy. What changed? One of the major factors contributing to this enormous surge in survival, can be attributed to the arrival of vaccines.
A vaccine is a combination of biological and chemical material which helps provide immunity to the body against several dangerous and deadly infections.
Vaccines work by training the immune system of the body to fight a specific pathogen, much before it actually attacks the body.
But how do you train the immune system to fight a pathogen, without causing the actual infection? The answer to this lies in understanding that the immune system doesn’t necessarily require an entire live pathogen to start a reaction towards it. Rather, it reacts to small molecules such as proteins and polysaccharides (sugars) present on the pathogen’s surface. Vaccine takes advantage of exactly this.
A vaccine essentially comprises either the entire pathogen (bacteria or virus), which have been weakened/killed, or several copies of specific molecules on their surface. Hence, when this is injected into the body, no infection is caused. Meaning these pathogens/molecules cannot reproduce and kill the body cells. However, the immune system still recognises these foreign agents and triggers an immune response against them.
So, what do we mean by an immune response? An immune response against any pathogen involves a cascade of events requiring several cells and molecules, ending with the activation of the B cells and the T cells. The B cells make millions of molecular missiles called antibodies. These specifically bind the foreign agent and target it for destruction. Most of the immune cells die soon after the infection is over. However specific types of cells called the memory B cells have a longer lifespan and remain behind. In case of a reinfection, these cells quickly recollect this infectious agent and trigger a much quicker response. They generate antibodies even before the establishment of an active infection.
However, many aggressive infectious agents can cause serious damage and even death, considering that the body takes a good amount of time to make antibodies (antibody production peaks at around 14 days). Hence a vaccine can be given before the prospective chance of an infection. This triggers the same immune response, ending in the production of memory B cells. If the actual infection strikes, the memory B cells quickly respond, making antibodies. Therefore the individual is now immunised against the infection.
A brilliant idea isn’t it? Wondering who the genius behind this was?
To be completely fair, the idea of creating a vaccine cannot be attributed to just one person. In fact, records from as early as the 15th century Chinese civilization, show how healed smallpox scabs from infected individuals were ground and blown into the nostrils of young uninfected children, in the hopes of immunising them against smallpox.
However, the invention of the first vaccine is commonly attributed to Edward Jenner. He used cowpox material to create immunity towards smallpox in the 16th century. In the coming centuries with the advancement in the understanding of medical science, scientists came up with vaccines against several deadly infections including - Rabies (Louis Pasteur in the 1800s), Measles (Maurice Hilleman in the 1900s) and most recently Polio (Jonas Salk in the 1900s).
As of today, vaccines have almost become a norm. The CDC recommends a whole list of common vaccines to be taken by children and adults based on their age. Although these vaccines produce the same ultimate outcome of triggering an immune response, the way they are made is quite different.
The ability of a pathogen to successfully enter and reproduce in a body, depends on the kind of molecules it contains. These could be surface proteins or polysaccharides, or specific toxins released by it. The immune system works by triggering a response against these molecules.
The design of a vaccine hence depends upon the kind of molecules that make up a given pathogen.
Weakened measles viruses are used in the vaccine against measles. © Sunaina Rao.
This variety of vaccine uses the actual live pathogen. However, it is hugely attenuated or weakened to a point that it is incapable of reproducing in the body.
Several vaccines including the ones for measles, mumps, rubella and chickenpox are made in this manner. In the case of the measles vaccine, live viruses originally obtained from sick patients are made to infect chicken cells grown in the lab. With repeated rounds of infection, the viruses become more and more efficient in infecting chicken cells, but in the process, become less efficient in infecting human cells. Now these viruses, although having very low or no ability to infect human cells, still have most of the structural proteins of their original selves. Hence they can be used to trigger an immune response without causing the disease or its symptoms. Therefore, the vaccine immunises the body against future attack by the actual pathogen.
These vaccines can produce a strong immune response, however since live viruses are used, it can cause the actual infection in individuals with weakened immune systems. Also there are chances the virus mutates back to its original unweakened form, however the probability of this happening is very low.
Dead polio viruses are used in the vaccine against polio. © Sunaina Rao.
These vaccines use pathogens which are inactivated by chemicals, heat or radiation.
Vaccines for polio, the seasonal flu and hepatitis A are made this way. In the case of polio, the viruses originally obtained from infected monkeys, are purified and concentrated, followed by inactivation using formalin. These viruses are absolutely incapable of causing an infection, but still contain all their structural proteins and can therefore initiate an immune response.
These vaccines are safer owing to the fact that the viruses used are completely inactive. However, as a result of this, the immune response generated isn’t strong enough. It requires booster doses to be administered, or needs to be injected with other immune enhancers.
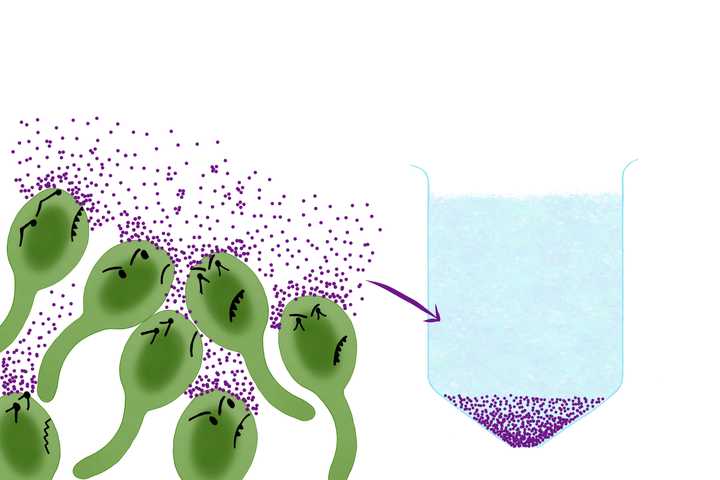
Tetanus bacteria - Clostridium tetani (green) releases the tetanus toxin (purple) which is used in the vaccine against tetanus. © Sunaina Rao.
Some bacteria, like the ones that cause diphtheria and tetanus, release specific toxins which are the main agents responsible for the disease. Vaccines for these bacterial infections can be made by extracting the toxins from the bacteria, followed by inactivating them to generate something called a toxoid - an inactivated toxin. This toxoid can now be injected to generate the required immune response.
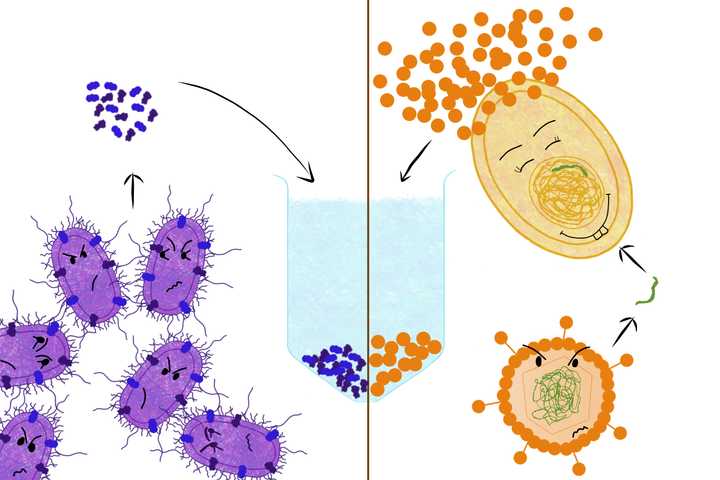
Left: Surface proteins are extracted from the whooping cough bacteria - Bordetella pertussis (purple) and used in the vaccine against whooping cough. Right: The gene (green) that codes for the protein - hepatitis B surface antigen (orange), is taken from the hepatitis B virus (orange) and incorporated into a yeast cell (yellow), which expresses the protein in abundance. This protein is used in the vaccine against hepatitis B. © Sunaina Rao.
Some vaccines are made using specific subunits of the bacteria or virus. These subunits may be proteins or other biomolecules that can generate a strong immune response. Hence no pathogen is used, just its bits and pieces.
An example would be the vaccine for whooping cough. Specific proteins from the causative bacteria (Bordetella pertussis) are extracted, and then injected into individuals to trigger an immune response. However massive amounts of bacteria would be required to obtain the required quantity of subunits. The solution? - recombinant DNA technology!
This technology has been used to generate the hepatitis B recombinant protein vaccine. Here, the gene that codes for a specific protein (hepatitis B surface antigen) is isolated from the hepatitis B virus and then incorporated into yeast cells. Yeast cells, unlike the virus, can be cultured in large amounts. These cells will now make the proteins on behalf of the virus, with each cell making thousands of copies. What better way to solve the previously mentioned shortage crisis?
However in the case of some bacteria, their surface polysaccharides which can be used as subunits, do not generate a strong enough immune response. In such cases, the bacterial polysaccharides are linked or conjugated to specific proteins that can generate a strong immune response. This is called a conjugate vaccine. The body, while generating an immune response against the protein, now also generates a response against the polysaccharide. An example for this is the vaccine for haemophilus Influenzae B, where the bacterial polysaccharide is linked to the tetanus toxoid protein.
Addressing the elephant in the room, are vaccines really worth taking? Have vaccinations made any difference at all and more importantly, are they safe?
The short answer to all these questions is - Yes, absolutely!
Let’s explore this in a little more detail. Data collected from different parts of the world suggest that vaccines have helped save millions of lives every year, with at least 10 million lives between the year 2010 and 2015. Smallpox, a savage killer of the past centuries has been effectively eradicated. Other deadly infections including polio, measles, mumps and rubella have been eliminated, if not eradicated in many regions of the world. Vaccinated individuals further prevent spread of the infection to the rest of the community, thereby protecting unvaccinated individuals as well. This type of immunity is called herd immunity. This should effectively answer if vaccines are really worth taking.
Are vaccines safe? Most of us must have heard the rumours on vaccines being linked to autism. For the ones who haven’t, a paper published in the journal - The Lancet in the year 1998, showed a link between vaccines and the occurrence of autism. This created a massive scare in the public, leading to several opting out of the vaccine. This in turn led to an increase in the cases of measles. However this paper was eventually heavily discredited for the several clinically unnecessary and unethical experiments performed. Further, no link has been found till date between vaccines and autism.
Moreover, vaccines undergo rigorous testing in the lab, in animal models, and human clinical trials before they can be licensed and marketed. Severe allergic reactions and death due to administration of a vaccine is not unheard of, however the chances of this happening is almost 1 per thousands to 1 per millions of doses. After all, no medicine is 100 percent risk free.
The bottom-line considering these statistics is that vaccines are amongst the safest medical products in use. In fact there are higher chances of one dying in a car crash than one would taking a vaccine! However by vaccinating ourselves, we save not just our life but also the lives of hundreds around us.