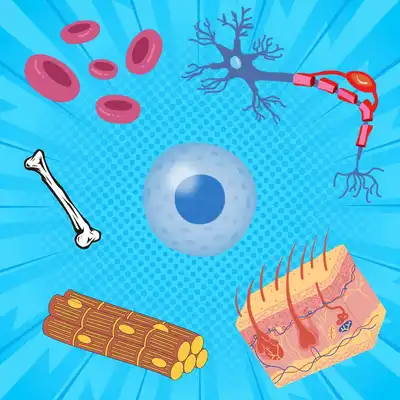
Everything you need to know about stem cells
What are stem cells, and what makes them so unique? What are the different types of stem cells, and how have they impacted modern medical science? Here is us answering all your questions about stem cells.

Medical science has come a long way when it comes to cancer treatment. Surgery, radiation therapy and chemotherapy were once the only treatment options available for cancer patients. Although these treatments control the progress of cancer to some extent, they are generic, targeting a broad range of cells and not just the cancer cells. They can therefore be low in efficiency and harsh at the same time.
However, with the advancement in medical biotechnology, we now have several therapies - some approved and some in the clinical trial stages, which help specifically target cancer cells. Cancer immunotherapy is one such therapy.
Cancer immunotherapy is a kind of treatment strategy that uses components of the immune system, like antibodies and the immune cells, to target tumour cells. The cells of our immune system continuously patrol different parts of our body, killing cancer cells as soon as they are born. However, cancer cells can develop suitable mutations that enable them to escape immune surveillance. Cancer immunotherapy mainly aims at strengthening the immune system by externally introducing components of the immune system into the patient’s body (Liu et al., 2022).
There are different types of cancer immunotherapy, one of the widely used among them being T cell therapy.
T cells are specialised immune cells in our body which play an important role in killing cancer cells. However, the rapidly dividing cancer cells can escape the T cells by a phenomenon called ‘immune escape’. T cell therapy therefore involves extracting T cells from the patient, expanding or culturing these cells in the laboratory, and reintroducing the cultured cells into the patient’s body. This thereby reinforces the patient’s T cells in attacking the tumour cells. Some T cell therapies also involve genetically modifying extracted T cells, making them more capable of targeting the cancer cells.
T cell therapies which involve the direct injection of the cells into the blood stream are widely used in the treatment of blood cancers, with several approved therapies and many in clinical trials. However, such T cells therapies have shown less efficacy in the treatment of solid tumours, one of the reasons being that the T cells need to specifically locate the solid tumour cells (Mirzaei et al., 2017).
A recent research published in the paper Nature Communications describes a unique technique to solve this problem (Adu-Berchie et al., 2023).
. Photograph of the rod shaped biomaterial made out of alginate and collagen. Credit: Adu-Berchie, K. *et al.*, 2023 [CC BY 4.0](http://creativecommons.org/licenses/by/4.0/).](/static/a03e9a69166f18075272918bd4dc32d4/b96f8/sivet.jpg)
Photograph of the rod shaped biomaterial made out of alginate and collagen. Credit: Adu-Berchie, K. et al., 2023 CC BY 4.0.
One of the main challenges with injecting T cells into blood circulation is that very few T cells actually reach the solid tumours. In order to solve this problem, the research group devised a unique biomaterial made out of alginate - a naturally occurring polymer found in seaweed, and collagen - a common structural protein found in our body.
. Electron microscopy image of the biomaterial showing its macroporous structure. Credit: Adu-Berchie, K. *et al.*, 2023 [CC BY 4.0](http://creativecommons.org/licenses/by/4.0/).](/static/2489127ed29e2957feb3059af44cb404/8e386/SIVET-SEM.jpg)
Electron microscopy image of the biomaterial showing its macroporous structure. Credit: Adu-Berchie, K. et al., 2023 CC BY 4.0.
The biomaterial was macroporous, meaning it contained several large pores. They added T cells and specific immune proteins called ‘APC recruitment factors’ into the pores of the biomaterial. The main job of these proteins was to activate specialised cells of the patient’s immune system called ‘antigen presenting cells’. They named this biomaterial SIVET (Synergetic in situ vaccine enhanced T cell depot).
It was hypothesised that the T cells in the SIVET would begin to kill the tumour cells. On the other hand, the APC recruitment factors would recruit additional cells of the patient’s immune system, called the antigen presenting cells, to the tumour site. The activated antigen presenting cells (ex. dendritic cells) would then travel to nearby lymph nodes and activate furthermore T cells in the lymph nodes, mounting an enhanced immune response against the tumour. They theorised, due to such heightened immune response, SIVETs would be more effective in treating tumours.
In order to test their hypothesis, they induced solid tumours in mice and conducted an experiment where they surgically implanted the SIVETs adjacent to the tumours. They then dissected the lymph nodes and the tumours from the mice after 14 days of treatment. They found that the tumours had an increased of immune cells, such as dendritic cells, when compared to the mice that were untreated.
The lymph nodes of the treated mice also contained an increased number of tumour reactive T cells. These results showed that, as hypothesised, the SIVETs were mounting an enhanced anti tumour response.
In order to check if the SIVETs had any positive effect in controlling tumour growth, they once again conducted a similar experiment and induced tumours in mice. SIVETs were then placed adjacent to the tumour and the tumour growth was monitored for more than 120 days. They found that the SIVETs significantly controlled the growth of the tumours, with some treated mice completely rejecting the tumour all together.
More interestingly, when additional tumours were introduced on the opposite side of the original tumour, one-third of the SIVET treated mice were able to reject this tumour as well. This indicated that the SIVETs had a long-lasting effect on tumour growth
The scientific community has faced several challenges when it comes to treating solid tumours using immunotherapy. Combining biomaterials with T cell therapy and immune proteins like APC recruitment factors, such as shown in this study, might take us a step forward in treating solid tumours like prostate, lung and pancreatic tumours. Additionally, SIVETs can easily be injected into the required location and therefore doesn’t require any invasive surgery.
Considering this ease of treatment and the efficiency, biomaterial based T cell immunotherapy might be the road to treating several complex solid tumours in the future.