Everything you need to know about stem cells
What are stem cells, and what makes them so unique? What are the different types of stem cells, and how have they impacted modern medical science? Here is us answering all your questions about stem cells.

We are surrounded by millions of microorganisms, which are just waiting for a chance to enter our bodies and cause an infection. It is indeed incredible that we do not fall sick too often. This is because we are equipped with a whole army of immune cells that immediately come into action when a microorganism enters our body. Two of the most important immune cells are the B cells and the T cells. The B cells are responsible for making proteins called antibodies that specifically bind and kill the microorganisms. The T cells, on the other hand, have the chief task of activating the B cells and also specifically killing the infected cells in our body. The key word here is ‘specificity’. In fact, the B and T cells undergo rigorous training to ensure they recognise and kill only foreign microorganisms and not the cells of our own body.
However, in some individuals, this specificity is broken. In such individuals, the immune cells mistakenly recognise the cells of their own body as ‘foreign’. This results in autoimmune diseases, where individuals start producing antibodies against their own cells, which can sometimes also be fatal.
Many types of autoimmune diseases have been observed in humans, and one of the most common among them is systemic lupus erythematosus (SLE) or Lupus.
. Patients with Lupus often show rashes on their skin. Credit: [Wikimedia](https://commons.wikimedia.org/wiki/File:Lupusfoto.jpg).](/static/07f5792c18e85cd142328fd1f59cb1ca/066f9/what-is-Lupus.jpg)
Patients with Lupus often show rashes on their skin. Credit: Wikimedia.
Lupus is a disease where the B cells start producing antibodies against certain molecules present inside the cell’s nucleus, for example, the DNA double helix. These antibodies are called autoantibodies, as they target one’s own cells.
Considering that patients develop autoantibodies against molecules that are present in every cell of their body, the result is a systemic disease. This means the disease can affect the entire body, typically involving the kidneys, nervous system, lungs, heart, skin, and the joints (Fava and Petri, 2018).
It is estimated that at least 5 million people across the world suffer from Lupus, mostly impacting women in the child-bearing ages.
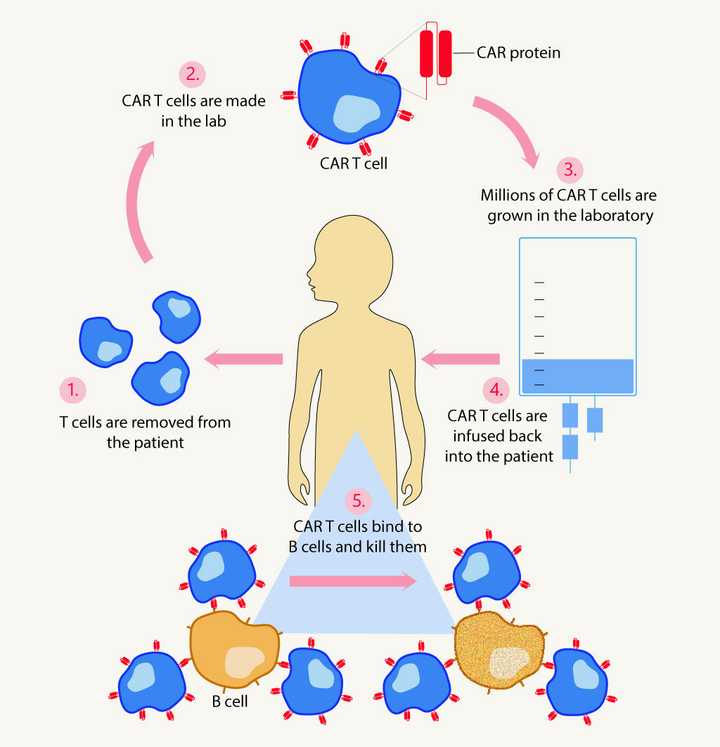
Steps involved in CAR T cell therapy: Step 1 – T cells are extracted from the patient. Step 2 – T cells are genetically modified so that they make a protein called the chimeric antigen receptor (CAR) protein on their cell surface. Step 3 – Millions of these CAR T cells are grown in the lab. Step 4 – These CAR T cells are infused back into the patient. Step 5 – CAR T cells specifically bind the B cells and kill them. © Sunaina Rao.
Today, there exists many state-of-the-art therapies to treat Lupus. Since the biggest problem in Lupus is the production of autoantibodies, most of the therapies aim to kill the patient’s B cells – the cells that make the autoantibodies. However, there are many patients who do not respond to these therapies, frequently resulting in organ failure and death.
A recent research work published in Nature Medicine explores a unique strategy in treating Lupus. The authors used specialised cells called CAR T cells to eliminate B cells (Mackensen et al., 2022).
What are CAR T cells?
CAR T cells or chimeric antigen receptor T cells are cells that are specifically designed to kill B cells. In order to create these cells, T cells are first extracted from the patient. These extracted cells are then genetically modified in the lab so that they make a protein called the chimeric antigen receptor (CAR) protein on their cell surface. Just like a key fits into a lock, these proteins fit into or ‘bind’ to specific proteins, present only on the surface of B cells. So, when these CAR T cells are reintroduced into the patient, they are able to specifically recognise and bind the B cells. Once bound, these T cells induce the death of the B cells.
Currently, there are many CAR T cell therapies that have been approved in the treatment of blood cancers – yet another disease that affects the B cells. Hence, the scientists in this study aimed to use a similar approach in treating Lupus.
In the current research, 5 Lupus patients – 4 women and 1 man, aged between 18 and 24 were studied. They all had active Lupus with multiple organs impacted like the kidneys, heart, lungs, and joints. The researchers extracted T cells from the patients and custom-made CAR T cells (as we discussed earlier) for each patient. These CAR T cells were then reintroduced into the patients. Thereafter, these patients were monitored to see the effect of the CART cells on their immune system.
Interestingly, all patients showed a rapid decline in B cells as well as autoantibodies after treatment. This therefore resulted in improved kidney, lung, and heart function. The scientists believe that CAR T cells might have the ability to kill off the B cells in blood circulation, as well as those present deep within tissues and lymph nodes. This is what sets it apart from the other B cell killing therapies.
More importantly, in long term follow-ups, they found that in all the patients the B cell count returned to normal, without any Lupus flare up. This was a relief, as B cells are very important for the body to actively defend itself against infections. The researchers think that the therapy might be rebooting the immune system, forcing the immune cells to function normally once again.
They believe that this could be a potential treatment for Lupus in the future. However, they also note that this is a small scale study and that the results must be seen with caution. We also need to wait and watch if these patients continue to be disease free over a long period of time.