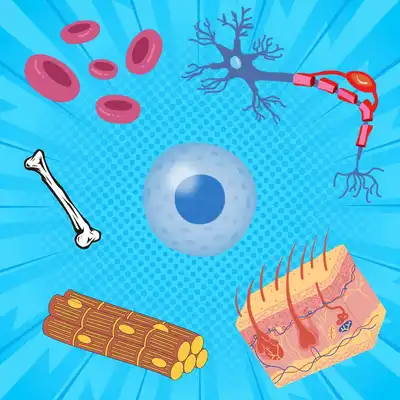
Everything you need to know about stem cells
What are stem cells, and what makes them so unique? What are the different types of stem cells, and how have they impacted modern medical science? Here is us answering all your questions about stem cells.

Invisible to the naked eye and microscopic in size, bacteria are present all around us, from the air we breathe to the food we consume. They reproduce in minutes and are constantly evolving newer and better ways to successfully infect us. Developing resistance to antibiotics is one of the several tactics used by bacteria to outsmart us.
Antibiotics are a class of medicines routinely used to treat bacterial infections. However, when bacteria are exposed to antibiotics over extended periods of time, they begin to evolve different ways by which they can escape the antibiotic. This means treating these resistant bacteria becomes increasingly difficult. This is called antibiotic resistance.
Based on a study published in the journal The Lancet, there were an estimated 4.95 million deaths associated with bacterial antibiotic resistance just in the year 2019 (Murray et al., 2022). Out of these, 1.5 million deaths were associated with lower respiratory tract infections, making it the most difficult to treat. Amongst the other infections that are becoming harder to treat due to antibiotic resistance are pneumonia, tuberculosis, gonorrhoea and foodborne diseases. Due to this, WHO and several other research groups agree that antibiotic resistance is a growing global concern and needs to be addressed urgently.
However, the first step in treating antibiotic resistance is understanding the mechanism by which bacteria develop resistance. A recent study published in npj Antimicrobials and Resistance explains one interesting mechanism (Trampari et al., 2023).
Bacteria contain specific proteins on their membrane which help expel molecules including antibiotics, toxins and other harmful substances from the cell to the outside. These are called efflux systems. The scientists involved in the study looked at a specific type of efflux system called AcrAB-TolC present in Enterobacteria, a family of bacteria that includes Escherichia coli (E. Coli) - the bacteria commonly found in our gut, and Salmonella - the bacteria known to cause typhoid. The AcrAB-TolC efflux system is a complex of three different proteins - AcrA, AcrB and TolC. These proteins work as a team and together help capture harmful substances and throw them out of the cell.
To study how these proteins help Salmonella in antibiotic resistance, they first cultured the bacteria under controlled laboratory conditions. They then exposed them to two common antibiotics - Azithromycin and Cefotaxime. After repeated exposure to these antibiotics, the bacteria evolved resistance to both the antibiotics. On examining the AcrAB-TolC protein complex in these resistant Salmonella cells, they found that the cells had undergone a very specific mutation in the AcrB protein. The cells exposed to Azithromycin developed a slightly different mutation in the AcrB protein when compared to the cells exposed to Cefotaxime.
When cells are exposed to antibiotics, the AcrAB-TolC protein complex bind to the antibiotic molecules and expel them out of the cell, similar to how a pump pumps out water from the inside of a tank to the outside. The group observed that the mutation in the AcrB protein brought about a change in the structure of the protein, thereby effecting the way in which it interacted with the antibiotic molecules. This difference in binding helped these proteins expel the antibiotic from the cell with greater efficiency.
Interestingly, the group were also able to identify isolates of Salmonella bacteria with this very mutation distributed in different parts of the world including the USA, UK, Ireland, Denmark and Bangladesh.
The research sheds light on the fact that all organisms are constantly evolving to become better and fitter versions of themselves. As humans devise newer, more effective antibiotics, bacteria too are evolving newer ways of combating these efforts. Understanding how bacteria develop resistance can take us one step closer to developing more efficient antibiotics and overcoming the crisis of antibiotic resistance.